Our approach is to use the advanced analytics, which can help the provider to identify and reduce fraud-related losses, as well as condense the claim cycle, which resulting in improved customer satisfaction. Our expertise team identifies procedure-to-diagnosis mismatches, unbundling occurrences, use of nonspecific diagnosis codes, global service violations, and many other problem areas that can adversely affect not just claims processing, but a provider’s overall practice. Our constant focus is on the claim submission date for claims follow-up and speed-up the AR to close all the claims balance based on Carrier adjudication time line.
HIPAA Compliant
Security & HIPAA
HIPAA (Health Insurance Portability and Accountability Act of 1996) is United States legislation that provides data privacy and security provisions for safeguarding medical information.
The security policy of Talluri Technologies ensures that all information security management requirements are noticed and are performing. We manages sensitive and vital corporate, customer information securely in addition to ensuring its confidentiality, integrity & availability. We have strong commitment in ensuring that the people, process and technology are secure.
Talluri operations and systems are HIPAA compliant. Utilizing our highly trained and skilled staff, ensure that our clients maintain the highest level of compliance.
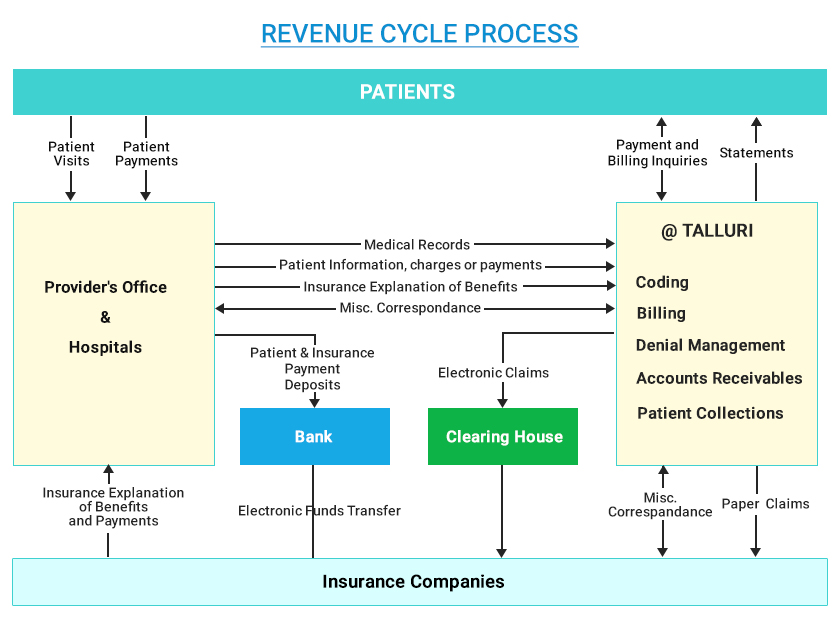
Revenue Cycle Process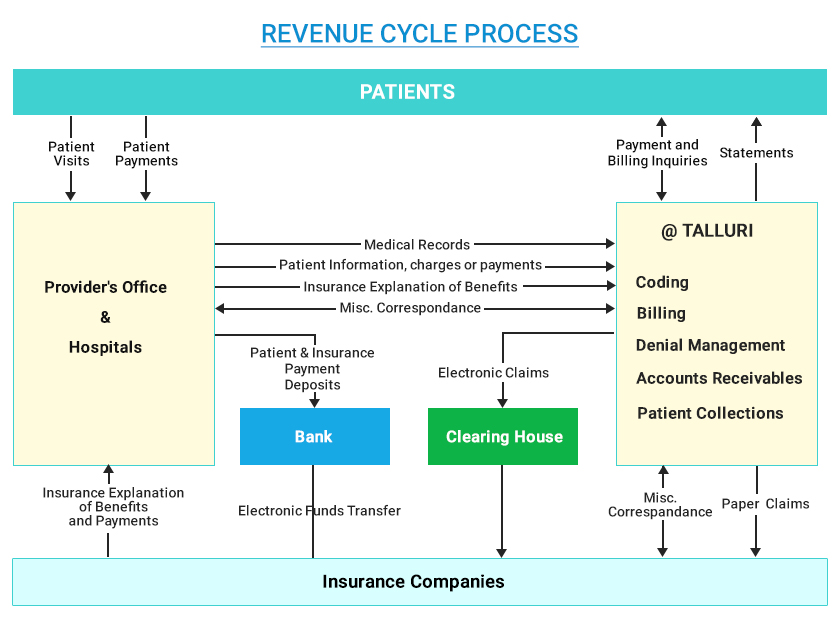
Revenue Cycle Process